Patient Opioid Notification Act (also called Opioid Patients Right to Know Act)
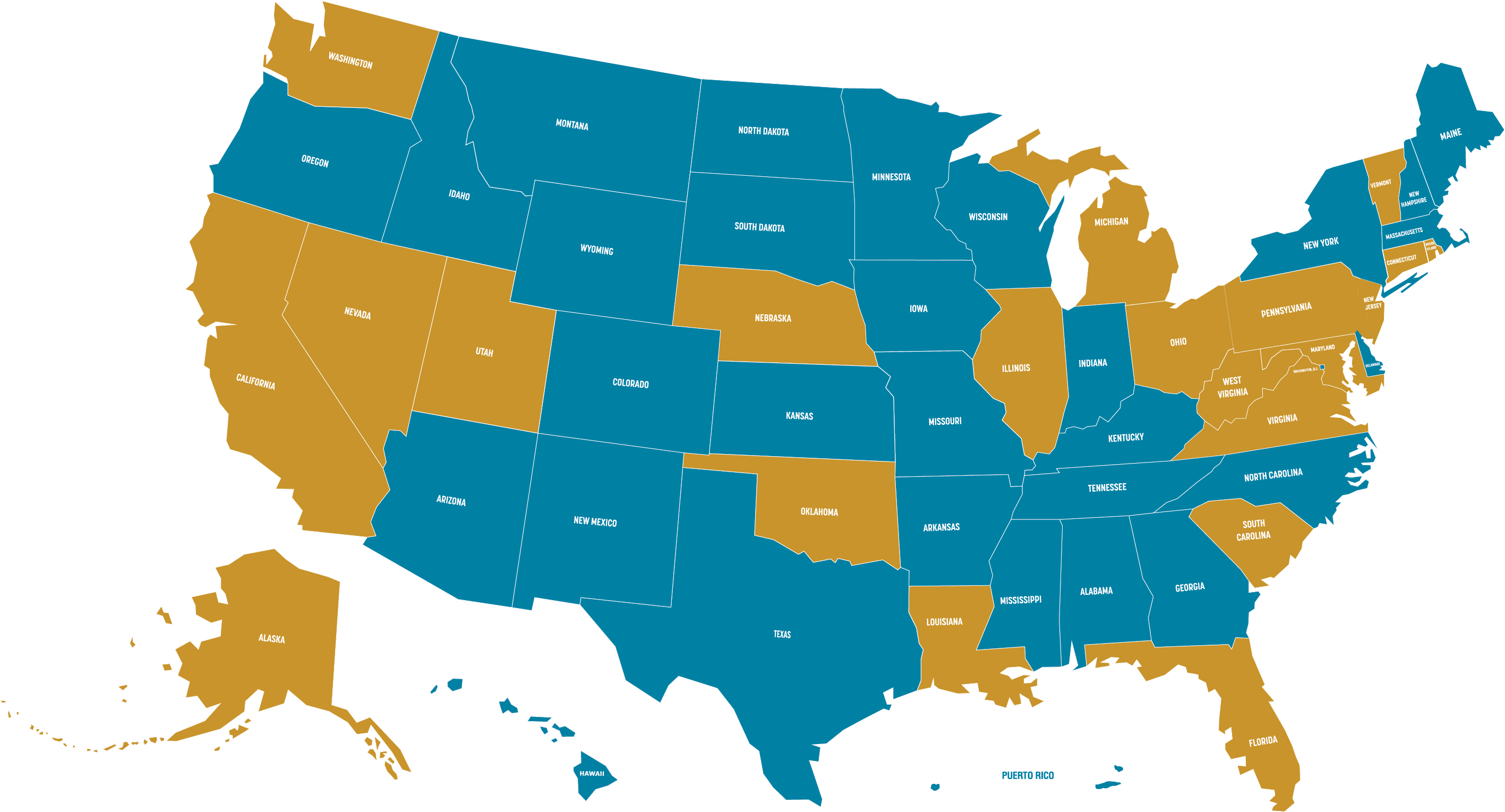
This common sense legislation, requiring a conversation between prescriber and patient before an opioid-based painkiller is prescribed and a discussion of potential alternative treatments when appropriate, is now law in, New Jersey, Rhode Island, Nevada, Maryland, Michigan, Oklahoma, West Virginia, California, Ohio, Connecticut, Utah, Washington, Louisiana, Nebraska, Pennsylvania, Florida, South Carolina, Illinois, Alaska, Vermont and Virginia as well as incorporated in the CDC guidelines for prescribing opioids. (In NJ, RI, MD, NV, OH, CT OK, WV, UT, WA, LA, NE, FL, IL, VT and VA, it applies across the board; CA, MI, PA, SC, and AK target it to youth and their parents.) Our goal is to make it the law in every state:
Click here to download a PDF of relevant pages of the New Jersey legislation, and the PDF of the comprehensive New Jersey preventing and treating opioid addiction law is here.
Sample adapted NJ language below:
d. Prior to issuing the initial prescription of a Schedule II controlled dangerous substance or any other opioid pain reliever which is a prescription drug in a course of treatment for acute or chronic pain and again prior to issuing the third prescription of the course of treatment, a practitioner shall discuss with the patient, or the patient’s parent or guardian if the patient is under 18 years of age and is not an emancipated minor, the risks associated with the drugs being prescribed, including but not limited to: (1) the risks of addiction and overdose associated with opioid drugs and the dangers of taking opioid drugs with alcohol, benzodiazepines and other central nervous system depressants; (2) the reasons why the prescription is necessary; (3) alternative treatments that may be available; and (4) risks associated with the use of the drugs being prescribed, specifically that opioids are highly addictive, even when taken as prescribed, that there is a risk of developing a physical or psychological dependence on the controlled dangerous substance, and that the risks of taking more opioids than prescribed, or mixing sedatives, benzodiazepines or alcohol with opioids, can result in fatal respiratory depression. The practitioner shall include a note in the patient’s medical record that the patient or the patient’s parent or guardian, as applicable, has discussed with the practitioner the risks of developing a physical or psychological dependence on the controlled dangerous substance and alternative treatments that may be available.
This section shall not apply to a prescription for a patient who is currently in active treatment for cancer, receiving hospice care from a licensed hospice or palliative care, or is a resident of a long term care facility, or to any medications that are being prescribed for use in the treatment of substance abuse or opioid dependence
Non-Opioid Pain Treatment Parity Act
It is essential that patients have access to affordable, quality non-opioid pain relief treatment. The Non-Opioid Pain Treatment Parity Act accomplishes this goal by requiring health insurers to provide the same level of coverage for effective pain relief alternatives as they do for opioids. It is often the case as blind pain studies confirm that a combination of ibuprofen and Tylenol is all that is needed. But in cases where physical therapy or one of the non-opioid prescription pain relievers, that are coming on the market, to name two examples, are called for, this legislation will ensure that they are well-covered by health insurance. Versions of this legislation have been adopted in Maine and Massachusetts. Provided below is the Maine version:
Sec. 1.
24-A MRSA §4311-A is enacted to read: §4311-A. Access to pain management services 1. Access to pain management services. A carrier shall develop a plan to provide adequate coverage of and access to a broad spectrum of pain management services, including, but not limited to, nonopioid, nonnarcotic medication for pain management and nonmedication pain management services that serve as alternatives to the prescribing of opioid or narcotic drugs in accordance with guidelines developed by the bureau. 2. Approval by bureau. A carrier shall file a plan required under subsection 1 with the bureau for approval. In its review, the bureau shall consider the adequacy of access to a broad spectrum of pain management services under the plan and whether any policies adopted by the carrier may create unduly preferential coverage of and access to prescribed opioids for pain management without consideration of other pain management services. 3. Information for enrollees. A carrier shall distribute educational materials to network providers about a pain management access plan under subsection 1 and post information about the pain management access plan on the carrier’s publicly accessible website.
Sec. 2.
Application. This Act applies to all policies, contracts and certificates executed, delivered, issued for delivery, continued or renewed in the State on or after January 1, 2026. For purposes of this Act, all contracts are deemed to be renewed no later than the next yearly anniversary of the contract date.
Sec. 3.
Appropriations and allocations. The following appropriations and allocations are made. PROFESSIONAL AND FINANCIAL REGULATION, DEPARTMENT OF Insurance – Bureau of 0092 Initiative: Provides a one-time allocation for a consultant to develop guidance on pain management plans. OTHER SPECIAL REVENUE FUNDS 2023-24 2024-25 All Other $0 $25,000 __________ __________ OTHER SPECIAL REVENUE FUNDS TOTAL $0 $25,000